Take Back Your Health (Part 4): Fat Versus Sugar
In Part 1 of this series, we explored what health is and which factors are driving the global burden of disease. In Part 2, we discussed why agency matters, where to begin, who to trust, and how to transform yourself from victim into agent. In Part 3, we analyzed why nutrition is our most direct pathway to health and investigated how we can apply food as medicine principles to our own lives. But we still haven’t answered one of the central questions relating to health:
What should we eat and how much?
This fundamental question has to do with the relationship between the 3 macronutrients: protein, fat, and carbohydrate. Of these 3, protein is the least confusing. We all know we need protein to survive, but the advice surrounding optimal fat and carbohydrate consumption continues to change.

More confusingly, diets demonizing one macronutrient or the other keep popping up and offering “secret knowledge” about how to lose weight and optimize health. Vegan and vegetarian diets espouse high-carbohydrate intake and demonize animal protein and fat, while advocates of paleo, ketogenic, and carnivore diets demonize carbohydrates.
Too much fat and protein (especially from an animal source) is frowned upon by medical authorities, and refined carbohydrates are readily available, require little time or energy to process, and generally seem to make life more simple and satisfying.
But taking the easy way out often has unforeseen consequences, and this holds true for both fat and carbohydrate consumption.
medical advice disclaimer: This website does not provide medical advice and is intended for informational purposes only. Any statements or claims about the possible health benefits conferred by any foods or supplements have not been evaluated by the Food & Drug Administration (FDA) and are not intended to diagnose, treat, prevent or cure any disease.

fat
Regardless of its poor reputation, fat is essential to human function. The human brain is nearly 60% fat, and cholesterol is a critical component of every mammalian cell. Without adequate fat consumption, a human being will sicken and die. So why has fat been increasingly associated with noncommunicable disease over the past century? The answer has more to do with politics and capitalism than it does with biology.
unsaturated fat
Unsaturated fats are found mostly in plants and are liquid at room temperature. Unsaturated fat is the only type of fat that is actively promoted by medical and political authorities. The healthiest types of these fats occur naturally in whole, unprocessed avocadoes, olives, nuts, seeds, and fish.

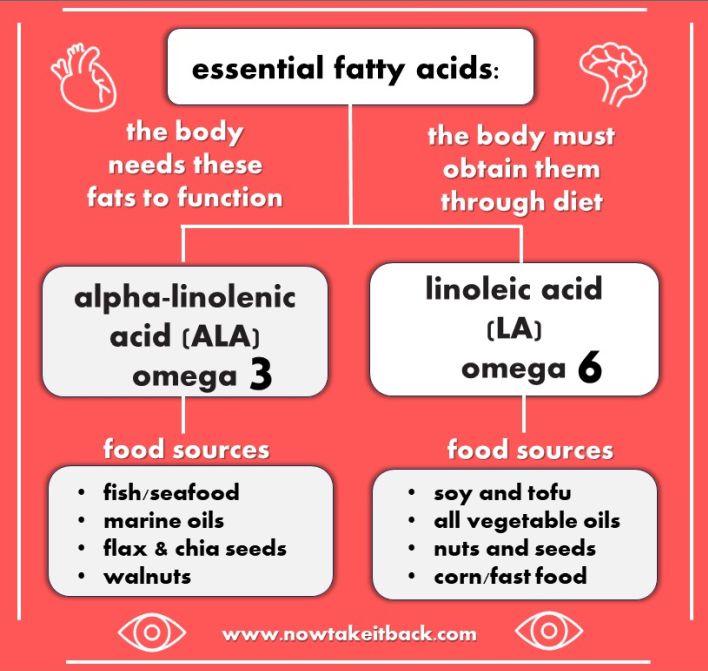
essential fatty acids
Essential fatty acids are polyunsaturated fats. They include alpha-linolenic acid (omega-3) and linoleic acid (omega 6). These fats are critical to brain, eye, and heart health; without adequate intake of omega 3 and omega 6, the brain, eyes, and heart will start to deteriorate. Moreover, the human body cannot produce these fats; it must obtain them from dietary sources.
Essential fatty acids are some of the only fats actively promoted by medical and political authorities. This is largely because without these fats, the human brain and body will sicken and die. However, omega 6s are promoted so heavily by authority and media that the ratio of omega-3 to omega-6 in the modern human diet has become radically disproportionate.
omega-6 to omega-3 ratio
Throughout human evolution, omega-3 and omega-6 consumption was approximately 1:1. Since the advent of processed food and the production of vegetable oils, omega 6 consumption has skyrocketed. This imbalance has contributed enormously to the burden of disease, particularly in the case of obesity. According to an article in Nutrients, today’s ratio of omega-6 to omega-3 consumption is roughly 20:1.
Too much omega-6 has been linked with infertility, breast cancer, and Alzheimer’s disease. Marketed as “heart healthy,” omega-6 consumption is effective at reducing blood cholesterol levels, but it simultaneously increases risk of death from heart disease:
[R]eplacing saturated animal fats with linoleic acid, an omega-6 polyunsaturated fatty acid, lowers serum cholesterol levels but increases the risk of death from coronary artery disease.
Canadian Medical Association Journal
Excess omega-6 intake is linked with both heart disease and cancer, the 2 leading causes of death in the United States. The primary sources of omega-6 in the American diet include: tofu/soy products, nuts and seeds, corn oil, fast food, and vegetable oil. Due to their inexpensive cost and shelf-stability, soy, corn, and vegetable oil are present in most types of processed/packaged food.

vegetable oil
Vegetable oil is the industrial byproduct of mechanically and chemically processing countless nuts, seeds, or legumes at high temperatures. These oils go through refining, degumming, deodorizing, bleaching, and purifying, causing nutrients to be lost and free radicals and trans-fats to be generated. Types of vegetable oil include sunflower oil, safflower oil, peanut oil, canola oil, corn oil, and soybean oil.
Vegetable oil is advocated as a healthy substitute for saturated/animal fat, and its consumption can be effective at lowering blood cholesterol levels. Its consumption is also effective at increasing omega-6 levels and predisposing the body to heart disease:
Omega-6 polyunsaturated fat linoleic acid promotes oxidative stress, oxidized LDL, chronic low-grade inflammation and atherosclerosis, and is likely a major dietary culprit for causing coronary heart disease, especially when consumed in the form of industrial seed oils commonly referred to as “vegetable oils.”
BMJ
Polyunsaturated fats (such as those present in nuts, seeds, and legumes) are chemically unstable, which means that they are easily damaged by heat, light, and oxygen. Because of this tendency to oxidize easily, polyunsaturated fats are difficult to preserve (think expensive bottles of olive oil in dark glass containers).

Vegetable oils are processed and refined using high levels of heat and oxygen. They are then marketed as “heart-healthy” for use in cooking, frying, and baking. The already oxidized oils oxidize further in home cooking, causing more nutrients to be destroyed and more free radicals and trans-fats to be created.
Thus, thermal oxidation changes the chemical structure of what begins as a healthy fat, causing it to become carcinogenic (cancer-causing). In this way, cooking with vegetable oil increases blood pressure and predisposes the body towards heart disease.
[I]ncreasing intake of high-linoleic vegetable oils and reducing that of animal fats . . . resulted in increased cardiovascular disease and all-cause mortality.
Pharmacology
canola oil
Canola oil is made from industrially crushed canola seeds. Canola was hybridized from rapeseed, a plant in the Brassica family with yellow flowers. Canola is marketed as “cholesterol free” due to its high content of polyunsaturated fat. Like other vegetable oils, canola oil loses its vitamin E, chlorophyll, and beta-carotene content during processing and oxidizes at high heat.

In mammal studies, canola oil has been found to increase body weight and decrease cognitive function, reduce antioxidant status, and increase bleeding times. More tellingly, chronic canola oil consumption shortens the life spans of stroke-prone spontaneously hypertensive (SHRSP) rats. Finally, all canola oil contains small amounts of trans fats, resulting from the process of refining and deodorizing.
Vegetable oils have been a lucrative achievement for humanity. They are not only edible; they have countless industrial applications in paints, lubricants, soaps, and biofuels. They cannot be made by the average home consumer; complex mechanical equipment is necessary. They are a gnostic solution offered by the food industry; they have succeeded in making the public believe we need their industrial product to obtain good health.
But if the convenience and widespread availability of vegetable oils are tipping the balance of omega-3 to omega-6 and predisposing the body towards heart disease, cancer, infertility, and Alzheimer’s disease, how can they possibly produce good health?
trans fats
Trans fats naturally occur in small amounts in animal fats and in large amounts in artificial fats, such as partially-hydrogenated vegetable oils. Natural trans-fats can be healthy in small amounts, while artificial trans-fats are toxic in any amount, but directly cause noncommunicable disease in large amounts.
artificial trans fats
The thermal oxidation that occurs during vegetable oil production results in the generation of a small amount of artificial trans fat residually present in most liquid vegetable oils. Artificial trans fats are mostly found, however, in partially hydrogenated oils or vegetable oils that have undergone a chemical process to make them solid at room temperature (i.e. margarine).
Artificial trans fats are highly toxic and found in ultra-processed and oxidized foods. Because they are cheap to produce, reusable, and filling, they are especially prevalent in restaurants. Foods high in artificial trans fats include:
- fried foods
- baked goods
- margarines
- vegetable shortening
- salad dressings

Artificial trans fat consumption has been found to cause nearly every type of noncommunicable disease.
Research has proved the direct connection of trans fatty acids with cardiovascular diseases, breast cancer, shortening of pregnancy period, risks of preeclampsia, disorders of nervous system and vision in infants, colon cancer, diabetes, obesity and allergy . . . trans fatty intake should be zero.
journal of food science and technology

Although the evidence is enough to suggest that artificial trans fatty intake should be 0, the Food and Drug Administration (FDA) allows food manufacturers to label their products as containing “0” grams of trans fats, as long as the trans fat quantity is less than .05 grams. This is how vegetable shortening products, such as the Crisco brand, are able to label themselves as “0 grams trans fat.”
natural trans fats
Many health authorities, including the World Health Organization, point out that trans fatty acids are present in the milk and fat of all ruminant (grazing) animals (i.e. cattle, sheep, and goat). These authorities cite studies that state that both natural and artificial trans fats raise blood lipid levels and consequently recommend limiting consumption of trans fatty acids to less than 1% of total energy intake.
However, a 2020 study in the International Journal of Molecular Sciences, entitled, “Dietary Fat and Cancer– Which is Good, Which is Bad, and the Body of Evidence,” states that the concentration of trans fatty acids in ruminant fat is roughly 6%, while the concentration of trans fatty acids in partially hydrogenated vegetable oils is up to 60%.

Additionally, another 2020 study from Advances in Nutrition, entitled “The Mechanisms of Action of Trans Fatty Acids,” states that although both natural and artificial trans fat consumption raises blood cholesterol levels, “only industrial trans fatty acids promote inflammation, endoplasmic reticulum stress, and cholesterol synthesis.”
Moreover, ruminant (natural) trans fats tend to appear as conjugated linoleic acid, which has been shown to have anti-obesity, anti-atherosclerotic (anti-heart-disease), and anti-cancer properties:
Conjugated linoleic acid (CLA), a fatty acid found naturally in ruminant animal food products, has been identified as a potential anti-obesogenic agent, with substantial efficacy in mice, and modest efficacy in obese human populations. Originally described as an anti-carcinogenic fatty acid, in addition to its anti-obesogenic effects, CLA has now been shown to possess anti-atherosclerotic properties.
Nutrients

Like all branches of science, lipid (fat) science is complex, nuanced, and constantly evolving. And yet, a consistent pattern in lipid science continues to emerge: industrially and artificially produced fats cause noncommunicable disease, while naturally occurring fats–from either plant or animal sources–protect against noncommunicable disease.
In the 1980s and 1990s, Dr. Mary Enig, a lipid scientist, worked to make the public aware that artificial trans fat–not saturated fat—caused heart disease. As a saturated fat with conjugated linoleic acid, butter has historically been implicated as a cause of heart disease; however, it is margarine—not butter–intake that increases the risk of coronary heart disease. And yet, despite the efforts of Dr. Mary Enig and many scientists like her, claims of the connection between saturated fat and heart disease remain adamant.
saturated fat
Saturated fats are found mostly in animals and are solid at room temperature. Animal sources of saturated fat include cream, butter, lard (pig fat), tallow (beef fat), and poultry fat (duck, chicken, goose, etc.) Plant sources of saturated fat include coconut, palm, and palm kernel oil.

For nearly a century, saturated fat has been accused of causing heart disease. This theory– which has now been disproven– began in the 1950s with a man named Ancel Keys.
lipid hypothesis
In 1958, American physiologist Ancel Keys launched his Seven Countries Study to research the relationship between diet and coronary heart disease. Keys is the original author of the lipid hypothesis.

In an article entitled, “To Err is Human: Can American Medicine Learn from Past Mistakes?”, author Jeffrey Ritterman states,
In 1978, Keys published his data in support of dietary fat as the cause of cardiovascular disease in the Seven Countries Study. Unfortunately, he excluded data from 15 countries and 4 indigenous tribes that did not fit well with his hypothesis.
Permanente Journal
The story behind why the lipid hypothesis became so pervasive and pernicious is told by authors such as Robert Lustig, in his book Fat Chance: Beating the Odds Against Sugar, Processed Food, Obesity, and Disease. The answer to such massive questions is often very simple: follow the money. Just as they did 80 years ago, food manufactures today continue to capitalize off the medical promotion of industrially-processed, highly-refined vegetable oils.
Based on flawed and incomplete data, the lipid hypothesis has long been disproven, but its cultural aftershocks are still being felt. Animal/saturated fat is still demonized, and industrial vegetable oil is still promoted as technology’s “healthy” solution.
The cholesterol-diet heart disease hypothesis is seriously flawed by statistical misinterpretation and faulty extrapolations from clinical trial studies. It should be allowed to pass into medical history.
cardiovascular engineering

cholesterol
Like saturated/animal fat, cholesterol has long been blamed as a cause of heart disease. As the body of evidence regarding how necessary cholesterol is to cell function, distinctions between “good” and “bad” cholesterol began to emerge as a way for medical and political authority to save face. These distinctions still hold sway, and primary care recommendations continue to be made to lower dietary cholesterol intake.
Cholesterol is essential to bodily health and integrity. The human brain cannot function without cholesterol. It is a critical component of every cell membrane and plays an important role in hormone development. Naturally low levels of cholesterol are correlated with poor cognitive function and increased risk of developing Parkinson’s disease.
Cholesterol is a major constituent in the mammalian body, serving as a functional and structural component of the cell membrane. Cholesterol is important for proper development of the nervous system and for hormone and vitamin synthesis in growing infants . . . Cholesterol acts as the major architectural component of compact myelin in this growth stage of life.
Nutricion Hospitalaria
Adequate cholesterol is necessary in both the beginning and end stages of life. One study found low maternal cholesterol levels to be associated with preterm delivery and increased risk of microcephaly (an abnormally small head in the newborn). Another study in The Lancet determined that in the very old (individuals over 85 years of age), higher cholesterol was linked with longevity.

Perhaps most concerning is the clear evidence that adequate cholesterol levels are needed for brain health. A study in Psychiatry Research states that low levels of cholesterol correlate with both aggressive and suicidal behavior in patients. A second study affirms,
[L]ower baseline cholesterol predicted external mortality (deaths from suicide, homicide, and accidents) and revealed an interaction with morbid depression.
Journal of Psychiatric Research
The link between normal-high levels of cholesterol and brain health is well-established. The link between normal-high levels of cholesterol and heart disease is not:
Recommending cholesterol lowering treatment based on estimated cardiovascular risk fails to identify many high-risk patients and may lead to unnecessary treatment of low-risk individuals.
BMJ
Although proven false many times over, the lipid hypothesis has led us to believe that saturated fat consumption/a high-cholesterol diet causes cholesterol to build up in the arteries, predisposing the body to heart disease. The science continues to accumulate regarding the body’s need for both dietary saturated fat and high-cholesterol foods, and yet this evidence receives little to no airtime in the media or medical propaganda.

causes of heart disease
According to the Centers for Disease Control and the World Health Organization, heart disease is the # 1 cause of death both in the United States and worldwide. It is so lethal that we have attempted to troubleshoot its development from every imaginable direction. Here’s a brief summary of what peer-reviewed scientific journals are stating about 5 of the potential culprits behind heart disease: saturated fat, cholesterol, artificial trans fats, vegetable oils, and sugar.

saturated fat?
A meta-analysis of [21] prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of coronary heart disease or cardiovascular disease.
American Journal of Clinical Nutrition
In findings counter to current beliefs . . . a diet very low in fat does not lower the risk factors for heart disease in healthy sedentary individuals and, in fact, may increase them.
University at Buffalo
National dietary guidelines were introduced in 1977 and 1983, by the US and UK governments, respectively, with the ambition of reducing coronary heart disease by reducing fat intake. . . To date, no analysis of the evidence base for these recommendations has been undertaken. . . There were no differences in all-cause mortality and non-significant differences in coronary heart disease mortality, resulting from the dietary interventions. . . Government dietary fat recommendations were untested in any trial prior to being introduced.
BMJ


cholesterol?
[R]eplacement of saturated fat with linoleic acid effectively lowers serum cholesterol but does not support the hypothesis that this translates to a lower risk of death from coronary heart disease or all causes . . . incomplete publication has contributed to overestimation of benefits, and underestimation of potential risks . . .
BMJ
A generally held belief is that cholesterol concentrations should be kept low to lessen the risk of cardiovascular disease. However, studies of the relation between serum cholesterol and all-cause mortality in elderly people have shown contrasting results. . . These data cast doubt on the scientific justification for lowering cholesterol to very low concentrations . . .
The Lancet
Elevated total serum cholesterol level, low HDL-C, and high total serum cholesterol to HDL-C ratio were not associated with a significantly higher rate of all-cause mortality, coronary heart disease mortality, or hospitalization for myocardial infarction or unstable angina . . .
JAMA


artificial trans fats?
The intake of trans fat has been associated with coronary heart disease, sudden death from cardiac causes, and diabetes.
New England Journal of Medicine
Saturated fats are not associated with all cause mortality, cardiovascular disease, coronary heart disease, ischemic stroke, or type 2 diabetes, but . . . Trans fats are associated with all cause mortality, total coronary heart disease, and coronary heart disease mortality.
BMJ
[I]ncreasing epidemiologic and biochemical evidence suggests that excessive trans fats in the diet are a significant risk factor for cardiovascular events as well as a risk factor for cancer and diabetes.
Diabetes and Metabolic Syndrome


vegetable oils?
Omega-6 polyunsaturated fat linoleic acid promotes oxidative stress, oxidized LDL, chronic low-grade inflammation and atherosclerosis, and is likely a major dietary culprit for causing coronary heart disease, especially when consumed in the form of industrial seed oils commonly referred to as “vegetable oils.”
BMJ
[I]ncreasing intake of high-linoleic vegetable oils and reducing that of animal fats . . . resulted in increased cardiovascular disease and all-cause mortality.
Pharmacology
[R]eplacing saturated animal fats with linoleic acid, an omega-6 polyunsaturated fatty acid, lowers serum cholesterol levels but increases the risk of death from coronary artery disease.
Canadian Medical Association Journal


sugar?
With both dietary fat and dietary cholesterol exonerated as causes of cardiovascular disease and type 2 diabetes, much recent research has focused on the role of fructose as a cause of these modern-day epidemics.
Journal of the American Academy of PA
This substitution of sugar for fat has been the major driver of the diabetes epidemic and has played a key role in causing coronary heart disease, strokes, fatty liver disease, obesity, hypertension, and some cancers.
Permanente
The Sugar Research Foundation sponsored its first Coronary Heart Disease research project in 1965. . . which singled out fat and cholesterol as the dietary causes of CHD and downplayed evidence that sucrose consumption was also a risk factor.
JAMA

sugar
There are many types of sugar, both natural and artificial. Naturally occurring simple sugars are found in milk, fruit, and honey. All carbohydrates, including those in vegetables, grains, starches, seeds, nuts, and legumes break down to glucose (a type of sugar) in the bloodstream.
Above, we discussed how naturally occurring plant and animals fats prevent disease, while man-made, industrialized fats cause disease. This also holds true for sugars/carbohydrates. Naturally occurring plant and animal sugars/carbohydrates prevent disease, while man-made, industrialized sugars/carbohydrates cause disease.
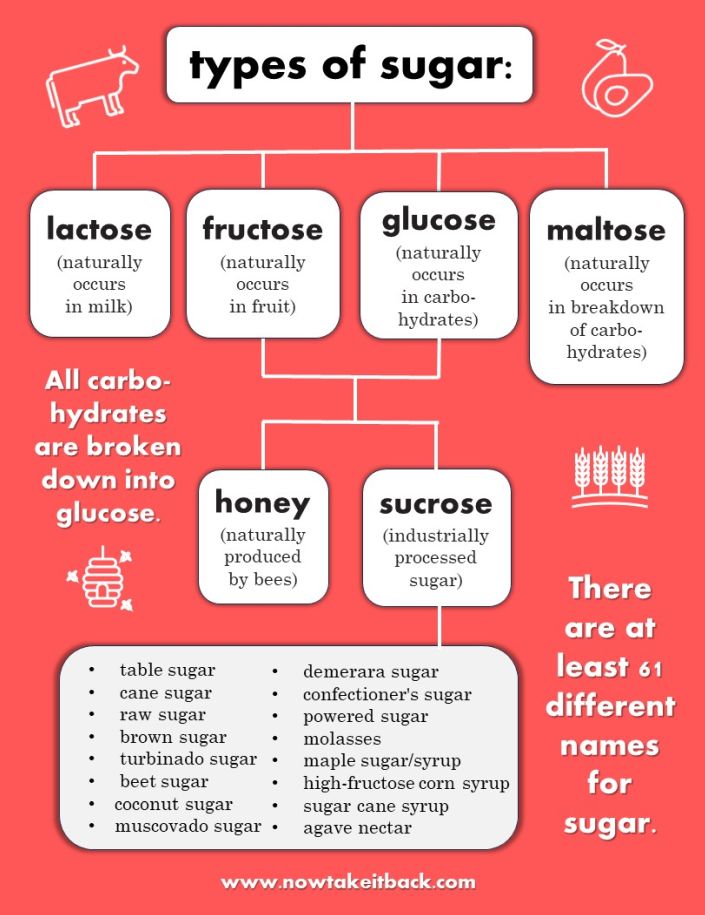
types of sugar
All forms of sugar are carbohydrates, and all carbohydrates break down into glucose in the body. The three naturally occurring forms of sugar are:
- lactose (simple sugars naturally present in milk)
- fructose (simple sugars naturally present in fruit)
- honey (simple sugars made by bees)
Sucrose is the chemical name for manmade, industrially-processed sugar. According to the University of California San Francisco Sugar Science team, there are at least 61 names for added sugar, which include:
- table sugar
- brown sugar
- molasses
- honey
- beet sugar
- cane sugar
- confectioner’s sugar
- powdered sugar
- raw sugar
- turbinado sugar
- maple syrup
- high-fructose corn syrup
- agave nectar
- sugar cane syrup
Added sugar is everywhere, especially in processed foods, whether bottled, bagged, canned, or jarred. Commercially available sauces, soups, salad dressings, beverages, and snacks all contain added sugars. A 2013 study from the The Journal of the Academy of Nutrition and Dietetics found that 74% of packaged food found in supermarkets contained added sugars.

To compound the problem of too much availability, sugar consumption is federally unregulated, and the recommended limits by the World Health Organization or the American Heart Association are typically unknown or ignored. As a result, most people consume too much sugar too frequently, without even realizing it.
Americans consume 57 pounds of added sugar each year, on average.
University of california san francisco sugar science
Part of the issue of overconsumption stems from the fact that sugar uses the same neurological pathways as opiates like cocaine. It is easily as addictive as alcohol and contains similar pain-relieving qualities. A 2002 study in Pediatrics found that although helpful in managing pain, sucrose analgesia for premature infants put those infants at risk for “poorer neurobehavioral development and physiologic outcomes.”
Because carbohydrates break down into glucose in the body, they have a similar drug-like effect on the brain as added sugars. A 2018 study in The British Journal of Sports Medicine found that sugar addiction causes “bingeing, craving, tolerance, withdrawal, cross-sensitization, cross-tolerance, cross-dependence, reward and opioid effects.” Like sugar, carbohydrate intake releases serotonin in the brain, causing feelings of temporary pleasure, followed by withdrawal, thereby creating a vicious cycle of dependence.

carbohydrates
Most medical authorities recommend a high-carbohydrate diet of fruits, vegetables, legumes, and whole grains. Much of the current “plant-based” movement is based on the flawed presupposition that if a food item is made only from plant materials, then it is superior in nutrition to animal foods.
High-carbohydrate diets can be healthy when they incorporate enough protein and fat. But high-carbohydrate foods such as legumes, whole grains, and vegetables require substantial processing to improve flavor and nutrition. This processing requires significant time and energy and is therefore often outsourced.
Commonly, high-carbohydrate diets do not consist of vegetables, whole grains, and legumes. Instead, fruit and nutrient-poor refined carbohydrates such as pasta, bread, cereal/granola, and energy bars dominate high-carbohydrate diets.

Refined carbohydrates release large amounts of glucose into the blood stream over long periods of time, contributing to conditions such as obesity and diabetes, both of which are risk factors for the development of heart disease and cancer, the world’s two most lethal diseases.
Low fat is seen as low calorie and therefore healthy, and there is little regard for the very real adverse effects of replacing fats, particularly saturated fats, with refined carbohydrate. Amongst this, saturated fatty acids appear somewhat victimised. A booming private market in processed “low fat”, high carbohydrate foods and spiraling obesity prevalence may be some of the legacy of such messages.
Journal of Primary Health Care
High-refined-carbohydrate diets impair cognitive function and predispose the brain towards neurological diseases such as Alzheimer’s, while high-fat and high-protein diets are associate with a reduced risk of cognitive impairment.

High-fat (also known as ketogenic) diets have also been found to be effective against cancer and epilepsy. Research has increased over the past 30 years regarding the gut-brain axis, a signaling pathway between the intestinal and central nervous systems. This research suggests a clear association between disorders of the brain and refined carbohydrate intake.
[T]he abusive consumption of refined, simple, and low-quality carbohydrates has a direct implication on the physical and mental pathophysiology. Then, carbohydrate consumption is postulated as a crucial factor in the development of the main Western diseases of the 21st century.
Nutrients
A diet high in simple and refined carbohydrates includes large quantities of fruit, pasta, bread, and other highly-processed grains or nuts. Whole grains, legumes, and whole nuts and seeds are complex carbohydrates with significant quantities of fiber, helping to balance glucose, insulin, and bowel function. A diet high in simple and refined carbohydrates and limited in complex carbohydrate predisposes the body to diseases such as Alzheimer’s and type 2 diabetes.

type 2 diabetes
According to the CDC, approximately 37 million Americans have diabetes, and approximately 90-95% of this 37 million have type 2 diabetes. According to the NIH, diabetes can lead to many diseases, including the two leading causes of death: heart disease and cancer. The global prevalence of diabetes has increased fourfold in the past 40 years.

More and more people are developing type 2 diabetes, including children and adolescents. Type 2 diabetes rarely occurs in isolation; it is often comorbid with obesity, dementia, and Alzheimer’s Disease.
Substantial evidence showing an association between type 2 diabetes and cerebral atrophy, cognitive impairment, and dementia is accumulating. . . High plasma glucose levels within the normal range . . . were associated with greater atrophy of structures relevant to aging and neurodegenerative processes, the hippocampus and amygdala.
Neurology
In fact, the neurodegenerative mechanisms of Alzheimer’s disease are so similar to those of diabetes that experts are now suggesting the term “Type 3 Diabetes” to apply to Alzheimer’s Disease.
Because high-refined-carbohydrate intake is a cause of type 2 diabetes, a high-fat, low-carbohydrate diet is beneficial for diabetic patients, and, in some cases, can cause remission of diabetes.

The increasing prevalence of both type-2 diabetes and Alzheimer’s Disease is directly attributable to the ubiquity, convenience, and availability of highly-processed sugary foods, beverages, and refined carbohydrates. However, it is also attributable to the dietary guidelines recommended by political and medical authorities.
dietary guidelines
Political and medical authorities recommend a high-carbohydrate and low-fat diet. The United States Department of Agriculture’s 2020-2025 Dietary Guidelines for Americans lists the following “core elements” of a healthy diet:
2020-2025 Dietary Guidelines for Americans, page ix
- Vegetables of all types—dark green; red and orange; beans, peas, and lentils; starchy; and other vegetables
- Fruits, especially whole fruit
- Grains, at least half of which are whole grain
- Dairy, including fat-free or low-fat milk, yogurt, and cheese, and/or lactose-free versions and fortified soy beverages and yogurt as alternatives
- Protein foods, including lean meats, poultry, and eggs; seafood; beans, peas, and lentils; and nuts, seeds, and soy products
- Oils, including vegetable oils and oils in food, such as seafood and nuts
Similarly, the USDA’s MyPlate (which replaces the old food pyramid) recommends that 50% of each plate should contain fruits and vegetables and at least another 25% should be grains (1/2 of which should be “whole”). This means that over 75% of every plate recommended by the USDA is primarily carbohydrates.

MyPlate additionally recommends low-fat protein and plant-based protein options, along with low-fat or fat-free milk, cheese, and yogurt, or fortified soy alternatives. Less than 25% of MyPlate is dedicated to fat and protein, and all recommended protein options are low-fat.
On page 3 of the 2020-2025 Dietary Guidelines for Americans, the introduction claims that these guidelines are “Grounded in Science and Focused on Public Health.” There are two questions worth asking in response to this claim.
- How is it possible for these guidelines to be “grounded in science” when the recommendations directly conflict with the conclusions of so many peer-reviewed studies?
- How is it possible for these guidelines to be “focused on public health” when rates of noncommunicable disease–especially heart disease, cancer, diabetes, and Alzheimer’s disease–continue to rise?
conflicts of interest
Both of these questions can be answered by the oppressive reality that many political and medical authorities are riddled with conflicts of interest that compromise both science and public health.

Conflicts of interest occur when an individual or institution’s actions contradict their mission or position. A conflict of interest constitutes a serious breach of ethics.
food industry
A March 2022 study in Public Health Nutrition entitled, “Conflicts of interest for members of the U.S. 2020 Dietary Guidelines Advisory Committee” sought to discover if the 2020-2025 Dietary Guidelines for Americans (cited above)–which are also the basis for MyPlate–were based on objective science and public health interest. The study reports the following:
Our analysis found that 95% of the committee members had conflicts of interest with the food, and/or pharmaceutical industries and that particular actors, including Kellogg, Abbott, Kraft, Mead Johnson, General Mills, Danone, and the International Life Sciences had connections with multiple members. Research funding and membership of an advisory/executive board jointly accounted for more than 60% of the total number of conflicts of interest.
public health nutrition
In other words, the public health experts who drafted the guidelines that Americans and medical authorities are supposed to follow to improve public health are being paid by food industry actors to recommend a high-carbohydrate diet that keeps Americans dependent on processed foods.


Processed food companies have sought to influence government policy, scientific studies, media, and education. The scope of their influence is directly linked to their revenues, which allow them to market aggressively, especially to children and low-and-middle income groups. According to the United States Securities and Exchange Commission, the Kraft Heinz Company alone earned revenues of $49.2 billion in 2010.
Processed food manufacturers have one central marketing goal: brand loyalty. Their objective is to convince buyers that their processed food products are nutritionally superior, highly convenient, readily available, and incomparable in taste. These companies will go to extreme measures to promote their products, even if it means paying to corrupt the conclusions of scientific research:
Food industry involvement in peer-reviewed research in leading nutrition-related journals is commonplace.
PlosOne

Food industries market aggressively to children through television and other media. Many studies have directly linked this unethical practice to the rise of childhood obesity. Additional studies have found that major food and beverage companies, including Nestle, Kraft, PepsiCo, and Danone, have “significant penetration” into low-and-middle-income countries where noncommunicable disease and disability are steadily rising.
Food and beverage companies use similar tactics to the tobacco industry to obscure science, suppress data, and influence public opinion. A study in The Lancet stated that dental health research organizations cannot produce meaningful research because of their conflicts of interest with the sugary food and beverage industries.
Food and beverage industries are intent on downplaying the emerging links between their products and noncommunicable disease. One of the primary NCDs caused directly by processed food and beverage industries is obesity.

beverage industry
In recent decades, an enormous amount of research has investigated the relationship between sugar-sweetened beverages (soda, juice, flavored water, energy drinks, etc.) and obesity. Concurrently, an enormous amount of money has been spent by the beverage industry to obscure and sideline this research.
A 2013 PLoS Medicine systematic review examined 18 studies on the relationship between sugar-sweetened beverages and obesity. This review found that authors with conflicts of interest with the food and beverage industries were 5x more likely to report no link or insufficient evidence of a link between sugar-sweetened beverages and obesity.

An investigation by The BMJ has uncovered evidence of the extraordinary extent to which key public health experts are involved with the sugar industry and related companies responsible for many of the products blamed for the obesity crisis through research grants, consultancy fees, and other forms of funding.
BMJ

Coca-Cola, in particular, has a lurid history of unethical behavior including product safety and health concerns. A study in the Journal of Public Health Policy found evidence that Coca-Cola had exchanged emails with the principal researchers of the the International Study of Childhood Obesity, Lifestyle and the Environment. These email exchanges “detailed exchanges on the study design, presentation of results and acknowledgement of funding.”
Food and beverage industries are not the only ones to benefit from corrupt nutritional advice that has made Americans sick and is keeping them sick. Pharmaceutical companies have profited obscenely from the opioid and obesity crises alike. With heart disease as the #1 cause of death nationally and globally, the pharmaceutical industries have rushed to the front with their own ubiquitous, profitable, and gnostic solution: statins.

statins
Statins are a class of medications that reduce the amount of cholesterol made by the liver. The most common side effect of statin use is muscle weakness, which, in a small portion of the population, can cause an often fatal muscle condition called rhabdomyolysis. Statins have also been shown to “disrupt insulin signaling pathways” and increase insulin resistance, thereby causing new-onset diabetes. Roughly 200 million people globally take statins, producing at least a 19 billion/year industry.
A bitter dispute has erupted
British journal of sports medicine
among doctors over suggestions that statins
should be prescribed to millions of healthy people at
low risk of heart disease. There are concerns that the benefits have been exaggerated and the risks have been underplayed. Also, the raw data on the efficacy and safety of statins are being kept secret and have not been subjected to scrutiny by other scientists.

The risk of new-onset diabetes with statin use is particularly high in postmenopausal women. In men, statin use can cause erectile dysfunction. As a preventative drug, statin therapy is expensive without clear evidence of being effective. Similar effort and funding to promote lifestyle changes to reduce heart disease risk has not been attempted. Rather, pharmaceutical companies pay physicians to prescribe brand-name statins to maximize profit:
[P]harmaceutical industry payments to physicians were associated with higher rates of prescribing brand-name statins. On average, a $1000 increase in total payments was associated with a 0.1% increase in the percentage of brand-name prescriptions.
JAMA INTERNAL MEDICINE
The risk-versus-benefit equation is difficult for any individual to negotiate, particularly in the case of prescription drugs. We often rely on political and medical experts to help us negotiate a realistic understanding of both risks and benefits when it comes to choices that impact our health and well-being. And yet, political and medical authorities lack consensus, are prejudiced by conflicts of interest, and seem motivated by everything except a sincere interest in public health.
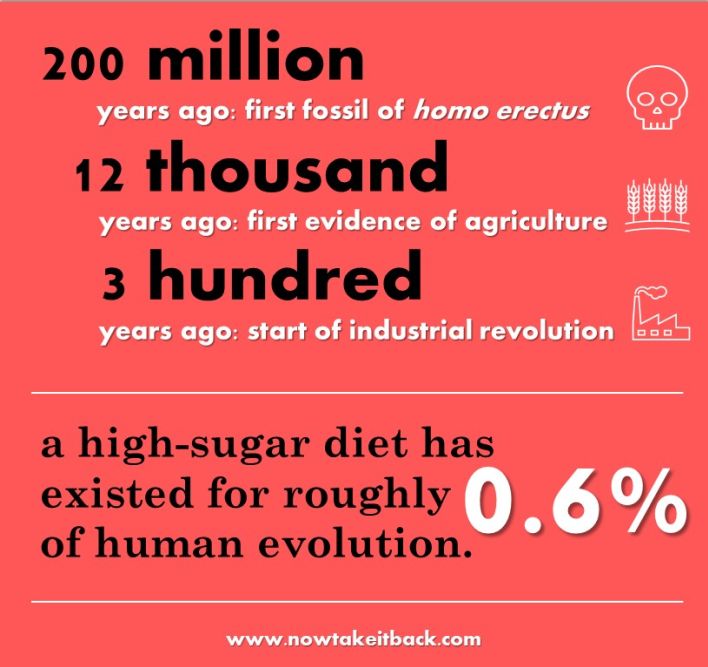
evolution
We know what the political and medical experts of today advise us to eat and what frequently drives this advice. But we can also gain insight from what evolutionary biology tells us about how our ancestors traditionally ate throughout the process of evolution.

Fossilized skulls of homo erectus date to roughly 2 million years old. During this time, early species of humans were hunter-gatherers, subsisting on animals that they either killed or scavenged. The size and complexity of the human brain is believed to have been fueled by high-quality animal foods, such as organs, blood, and fat. In his book, Eat Like a Human, food archaeologist Bill Schindler supports this theory:
[H]igh-quality animal fat literally helped fuel our most profound evolutionary advances as humans. Humans began eating meat by scavenging from dead animals whose viscera—the organs, blood, and fat—had already been stripped by predators. It took another 1.5 million years for us to develop the technology to hunt, and only then, after we were the first to a kill and were regularly eating the most nutritious parts, did our brains and bodies begin to grow exponentially.
Bill schindler, eat like a human, pg. 63
It is also believed that early hominids gathered carbohydrates such as edible roots and tubers as a dependable source of energy. Cooking technology enabled humans to maximize and access nutrition in both animals and foraged plants and therefore played a critical role in the growth of the human brain. Despite some evidence of early carbohydrate consumption, human cultivation of edible plants did not begin until very recently in the 2 million-year-old history of homo erectus.

The origins of agriculture date to approximately 12,000 years ago. This means that human genetics only began to adapt to a more diverse range of carbohydrate intake in the recent evolutionary past. In other words, the advent of agriculture represents 0.6% of the total evolutionary time of homo erectus.
Large-scale food production and processing did not begin until the Industrial Revolution, some 300 years ago. To put this in perspective, humans have been eating processed food for 0.015% of the total evolutionary time of homo erectus.
evolutionary discordance
The theory of evolutionary discordance argues that human genes have not had enough time to adjust to an agriculture-based diet, more or less the highly processed and industrialized foods of the past few centuries.
There is growing awareness that the profound changes in the environment (eg, in diet and other lifestyle conditions) that began with the introduction of agriculture and animal husbandry approximately 10,000 years ago occurred too recently on an evolutionary time scale for the human genome to adjust.
American Journal of Clinical Nutrition
The carbohydrates of the past 2 million years are not the carbohydrates of the past 12,000 years. From an evolutionary perspective, the taste of sweetness triggered early humans to consume as much quick energy as possible, thereby fueling the more physically taxing pursuit of nutrient-dense food, such as killing and cooking an animal.

Naturally-occurring sugars in fruit were only available to our ancestors seasonally, and honey was highly protected by bees. With the advent of agriculture, humans began to hybridize many plants to increase sugar content and thereby the taste of sweetness.
With the advent of refined carbohydrates, the taste of sweetness continued to grow exponentially, thereby leading to addiction. In a PLOS One article entitled, “Intense Sweetness Surpasses Cocaine Reward,” the authors concluded:
In most mammals, including rats and humans, sweet receptors evolved in ancestral environments poor in sugars and are thus not adapted to high concentrations of sweet tastants. The supranormal stimulation of these receptors by sugar-rich diets, such as those now widely available in modern societies, would generate a supranormal reward signal in the brain, with the potential to override self-control mechanisms and thus to lead to addiction.
PLOS One
The theory of evolutionary discordance argues that such a rapid shift towards increased carbohydrate and sugar-rich foods has caused the human genome to react with disease and addiction. This theory is further supported by the traditional diets of indigenous populations, such as the African Maasai and Arctic Inuit.
traditional diets
The Maasai of East Africa are a hunter-gatherer tribe who live and eat much the same way as their ancestors have for thousands of years. Their economy is based on their herds of sacred cattle, upon which they rely for food, clothing, and shelter. The Maasai diet is largely based on consumption of milk and dairy products, meat, cattle fat, and blood, from which they derive their salt intake.

“Several studies have revealed that the Maasai, pastoralists in Tanzania, have low rates of coronary heart disease despite a diet high in saturated fat.”
British Journal of Sports Medicine
The Arctic Inuit are indigenous people living in northern Canada, parts of Greenland, and Alaska. The traditional Inuit diet is based almost totally on marine meat and fat, with little to no plant or carbohydrate consumption. A study of East-Greenland traditional nutrition found that the native diet was comprised of 41% protein, 49% fat, and 10% carbohydrate. The introduction of refined carbohydrates to this population is believed to have caused an increase in dental caries, hypertension and atherosclerosis.

“In the 1970s the preventive effect of marine fat on cardiovascular disease, thrombosis and atherosclerosis was described. The low incidence of ischemic heart disease among Greenlanders has been related to the high intake of marine food.”
Many traditional diets support the evolutionary discordance theory and challenge the lipid hypothesis. The “French Paradox,” which states that the French have extremely low rates of heart disease despite a diet high in saturated and animal fats, represents yet another example. In her excellent book, Deep Nutrition, Catherine Shanahan describes the role that animal protein and fat play in traditional diets across the world:
Until around 1940, the Netsilik Eskimo traditionally ate seal, fish, lichen, and not much else. In the Mongolian desert today, nomadic bands of camel breeders eat mainly dairy products, some grains, lots of tea, root vegetables, and meat. In the rain forest of Papua New Guinea, one of the last surviving hunter-gatherer groups, the Kombai, dine on fat grubs of giant flies, lizards, birds, pounded sago palm hearts, and—for special occasions—fattened pig. In West Africa, farmers known as the Mofu grow millet, beans, and peanuts, forage for insects, and raise goats and chickens, just as they have for thousands of years.
Catherine Shanahan, deep nutrition, pages 239-240
As Shanahan outlines so thoroughly in Deep Nutrition, none of these indigenous peoples eat a diet dominated by vegetable oils, trans fats, or sugar. And when these heavily processed “foods” are introduced to indigenous populations, the rates of noncommunicable disease increase radically.
Evolutionary biology, natural law, and modern science all offer evidence that the human attempt to render the work of producing and processing food more economical and efficient has severely backfired into pandemic levels of noncommunicable disease. In almost every aspect of human life, taking the easy way out has unforeseen and damaging consequences, and food production and processing is no exception.

fat versus sugar 101
The controversy surrounding fat versus sugar is one of the most basic questions facing us as parents. It’s a question that impacts the food we choose to consume and to give to our children every single day. It’s a question that impacts every dimension of our health and directly influences our susceptibility to noncommunicable disease.
It’s impossible to know the absolute truth, but all the evidence seems to boil down to 3 critical points:

1. Highly processed and refined fats (such as liquid and partially hydrogenated vegetable oils) cause noncommunicable disease.

2. Highly processed and refined carbohydrates (such as cereals, breads, crackers, cookies, and sugar-sweetened beverages) cause noncommunicable disease.

3. Nutritional advice from political and medical authorities is compromised by conflicts of interest.
If these 3 statements are true, then there is only one path forward:
Do not eat any food you haven’t processed yourself.
This sounds simple, but learning how to process all of your own food– especially when you’re not used to it–can feel overwhelming at first. Just remember the principles of true growth discussed in Part 3 of this series:

lasting change comes slowly, over time
try to learn only one new thing at a time
make time for rest and integration
practice a new skill until you gain confidence
you only fail when you stop trying
It’s also useful to remember the 90/10 rule:
If you make a habit of eating whole foods that you process yourself 90% of the time, your body will be able to sustain special occasions or crazy busy days.
Be gentle with yourself, and take it one step at a time. I’m here to help.
about my 101 series
My 101 Series empowers parents to inform themselves prior to making decisions that can have lifelong consequences. Each 101 e-book contains 101 fully cited facts towards either informed consumption or informed consent regarding a controversial topic.
I source each fact from either an established medical authority, published authors with serious credentials, or published, peer-reviewed studies from PubMed, the National Library of Medicine’s free online database.
Each fact is either hyperlinked or the page number of a particular book and author is included in parentheses following each quote. A bibliography and a complete list of online sources are both included at the end.
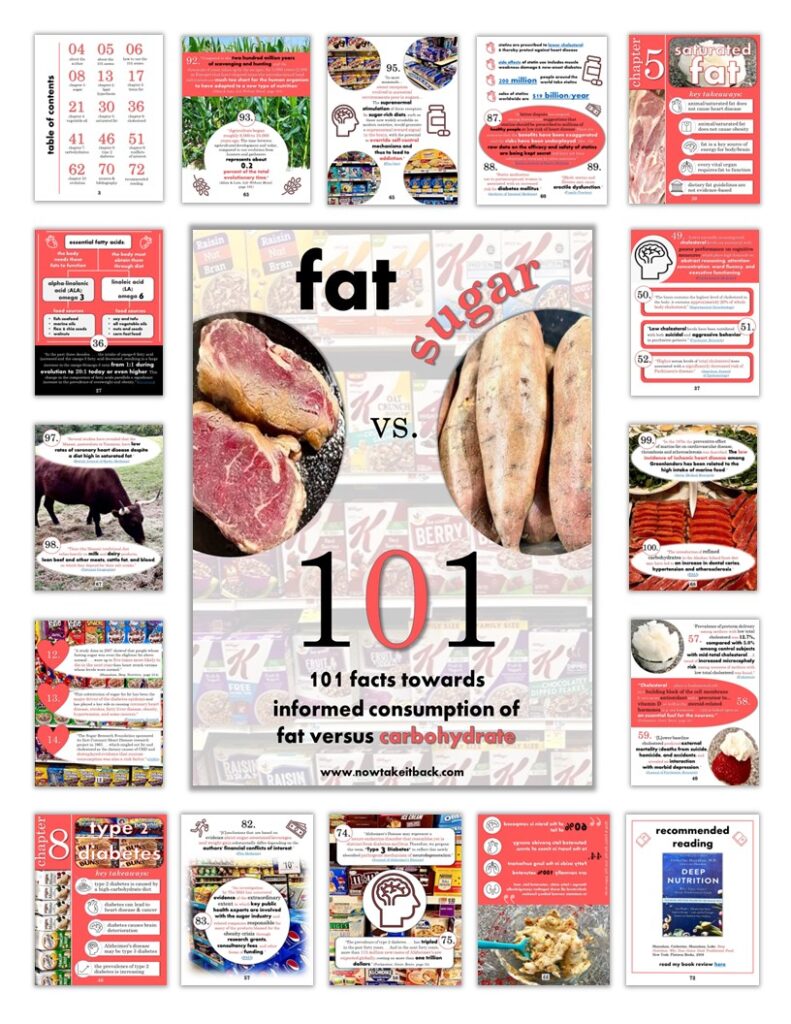
how to use my 101 Series
Most modern controversial topics regarding physical or mental health are heavily slanted towards the broad consensus of medical or political authorities, even when those authorities have been found to have serious conflicts of interest. Because these authorities have a larger scope of influence and funding, they often promote information (or misinformation) that can sometimes border on propaganda.
My 101 Series is intended to balance the equation by highlighting the legitimate science that isn’t often covered by the media. It distills highly complex topics into digestible and practical information with clear source citations for further research. In this way, my 101 Series serves as a launching point for parents to deep-dive as far as they wish.
My goal is to help make research that properly belongs to parents more accessible, understandable, and actionable. I hope to empower parents to begin trusting their own judgement over the advice of authorities that may–or may not--have their children’s best interests at heart.
My goal is not to pretend I have the answers. Instead, I want to promote the scope and the gravity of the issues modern parents face. I want to help parents equip themselves with the knowledge and information they need to make truly informed choices for their children. To foster in themselves both awareness of the freedom to refuse and viable alternatives. To take the responsibility for their family’s health back into their own hands. To take back self-education and self-advocacy.
And, in the process, transform themselves from victim into agent.


Unless effective population-level interventions to reduce obesity are developed, the steady rise in life expectancy observed in the modern era may soon come to an end and the youth of today may, on average, live less healthy and possibly even shorter lives than their parents.
“A Potential Decline in Life Expectancy in the United States in the 21st Century”
If you are unwilling to accept this prognosis for yourself and your family, subscribe below to begin taking control of your life.
take my free 5-day challenge
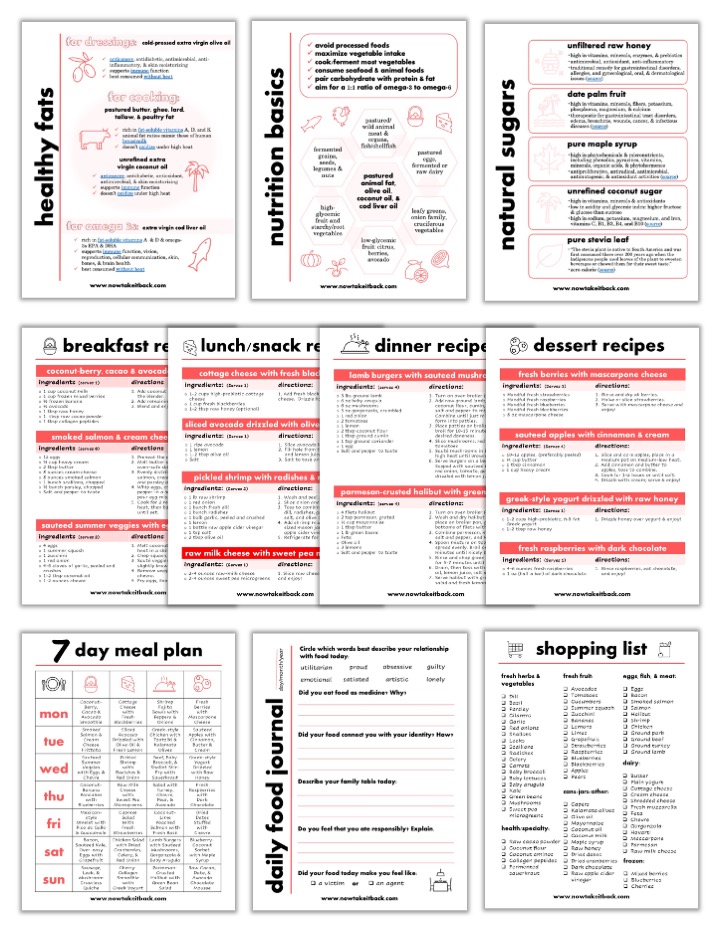
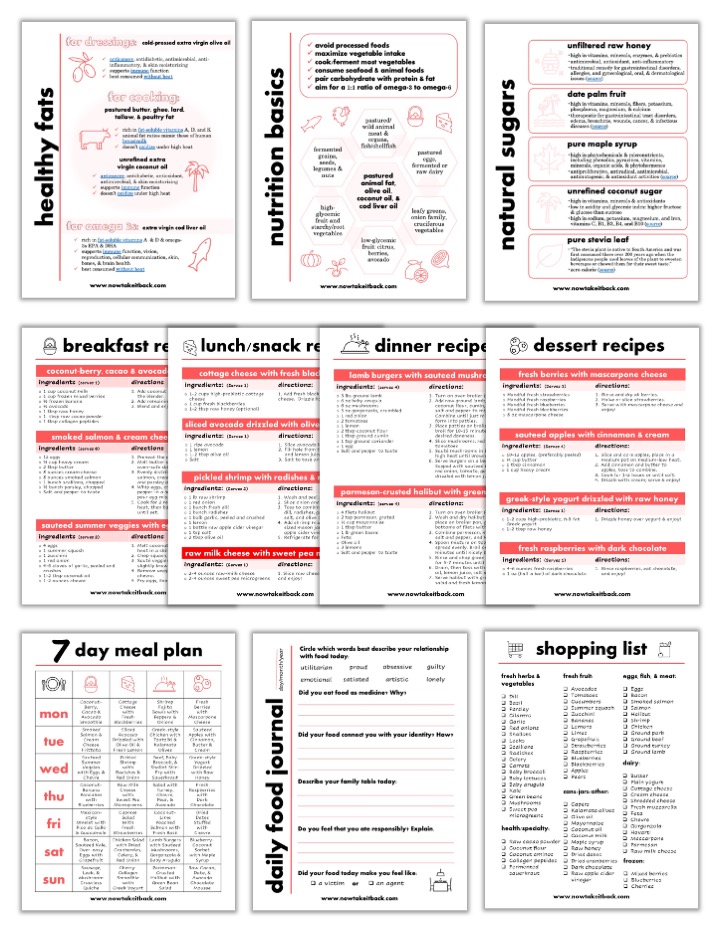
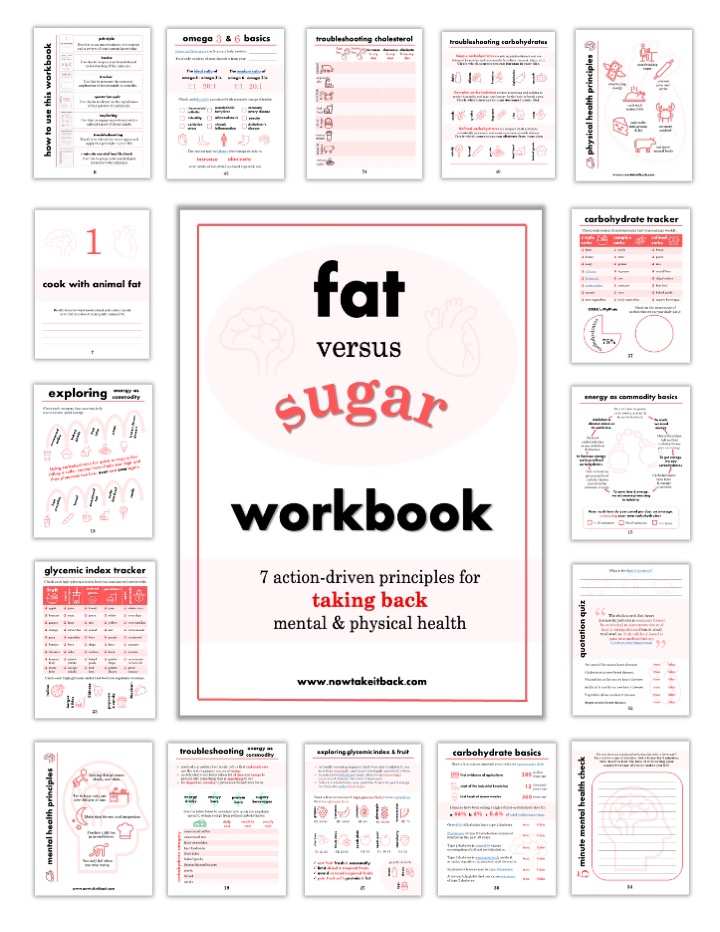
& instantly access: